Introduction:
Hemophagocytic lymphohistiocytosis (HLH) is a severe hyperinflammatory syndrome caused by the abnormal activation of macrophages and T cells. The primary form, resulting from lymphocyte-related mutations, is more common in children, while the secondary (acquired) form known as sHLH prevails in adults. sHLH is often triggered by infections or malignancies (Mal-HLH) but can also be induced by autoinflammatory disorders called macrophage activation syndrome (MAS; or MAS-HLH). We present a retrospective case series of adults treated for sHLH at a single institution from 2012 to 2023.
Methods:
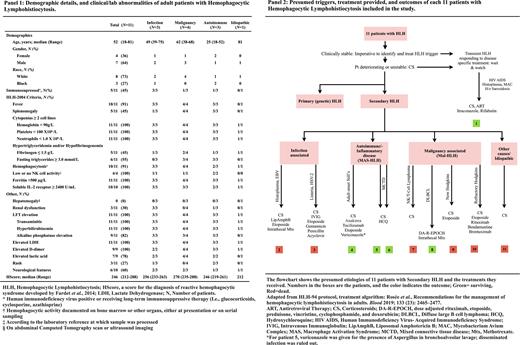
Retrospective data was collected using the EDW database, and 36 patients were identified using ICD 9/10 codes 288.4 and D76.1 for HLH. Subsequently, a manual review of electronic medical records was conducted; criteria for inclusion were age >18 years at the time of diagnosis and meeting HLH-2004 criteria ( Panel-1).
Results:
Out of the 36 patients reviewed, 11 met the criteria and were included in the analysis. These cases occurred between 2015 and 2023. The median age at diagnosis was 52 (range 18 to 81). The female-to-male ratio in our study was 4:7. Most patients (73%) were white. Additionally, 45% of the patients were immunocompromised.
91% of the patients presented with fever, while only 45% had splenomegaly. Trilineage cytopenias were observed in all patients. In our study, 5/11 had hypofibrinogenemia, and 6/11 had hypertriglyceridemia. Hemophagocytosis was evident in 91% of the patients. Natural Killer (NK) cell activity was measured in 4 patients, and all exhibited low or no NK cell activity. In 10 out of 10 patients, soluble IL-2 receptors were elevated.
None of the patients in the study had hepatomegaly, but all had transaminitis and hyperbilirubinemia, and 82% had elevated alkaline phosphatase levels. Elevated lactate levels were observed in 78% of patients, and 27% had a rash. Neurological features were observed in 6 out of 10 patients. Lactate dehydrogenase was elevated in all patients with a median value of 1551 U/L (range 354 - 3689)
Presumed etiologies for sHLH included malignancy (4), infection (3), autoimmune disease (3), and unknown cause (1). Treatment was highly individualized based on the underlying trigger and was guided by the HLH-94 protocol ( Panel-2). All patients received high-dose steroids, 6/11 received etoposide, and 2 received intrathecal therapy for neurological involvement.
Conclusion:
At a median follow-up period of 16 days, five patients had died. The survival rates at 30 days and 1 year were 45% and 27%, respectively. The overall mortality rate was 55%. While mortality rates were 75% in the Mal-HLH arm and 67% in the infectious arm, all patients with MAS-HLH survived while performing the study indicating a better prognosis for patients with this type of HLH.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal